Depression and Antidepressant Drugs
- What is Depression?
- Symptoms of Depression.
- Possible mechanisms behind
Depression.
- Drugs used for the treatment of
Depression.
What is Depression
Depression (major depressive disorder) is a common and serious medical illness that negatively affects how you feel, the way you think, and how you act. Depression is the most common of the affective disorders (defined as disorders of mood); it may range from a very mild condition, bordering on normality, to severe (psychotic) depression accompanied by hallucinations and delusions. It is a mental disorder, in which the patient is characterized by pervasive and low mood with low self-esteem and the patient may lose interest in daily social life and activities, sad mood, tiredness, guilt, sense of worthlessness, lack of concentration, and suicidal thoughts. Worldwide, depression is a major cause of disability and premature death.
In addition to the significant suicide risk, depressed individuals are more likely to die from other causes, such as heart disease or cancer. Depression is a heterogeneous disorder, with patients presenting with one or more core symptoms, and depression is often associated with other psychiatric conditions, including anxiety, eating disorders and drug addiction.
Symptoms of
depression
The symptoms of depression include emotional and biological components.
Emotional symptoms include:
• low mood, excessive rumination of negative thought, misery, apathy and
pessimism
• low self-esteem: feelings of guilt, inadequacy and ugliness
• indecisiveness, loss of motivation
• anhedonia, loss of reward.
Biological symptoms include:
• retardation of thought and action
• loss of libido
• sleep disturbance and loss of appetite
Type of depression
There are two distinct types of depressive syndrome, namely unipolar depression, in which the mood changes are always in the same direction, and bipolar disorder, in which depression alternates with mania.
1. Unipolar depression is commonly (about 75% of cases) non-familial, clearly associated with stressful life events, and usually accompanied by symptoms of anxiety and agitation; this type is sometimes termed reactive depression. Other cases (about 25%, sometimes termed endogenous depression) show a familial pattern, unrelated to obvious external stresses, and with a somewhat different symptomatology.
2. Bipolar disorder, which usually appears in early adult life, is less common and results in oscillating depression and mania over a period of a few weeks. It can be difficult to differentiate between mild bipolar disorder and unipolar depression. Also, bipolar manic episodes can be confused with episodes of schizophrenic psychosis.
However, the exact cause is still not known. It can be caused by any change in neurotransmitter levels such as changes in Norepinephrine, Serotonin, Dopamine etc. and it can also cause by any physical or environmental factor. Genetics of a person also cause depression as some have a family history of depression they are more prone to have depression.
Different
Theories of depression
1.
THE MONOAMINE THEORY
2.
NEUROENDOCRINE MECHANISMS
3. TROPHIC EFFECTS AND NEUROPLASTICITY
The main PR depressive
pathways involve the hypothalamic–pituitary–adrenal axis, which is activated by
stress and in turn enhances the excitotoxic action of glutamate, mediated by
NMDA receptors, and switches on the expression of genes that promote neural
apoptosis in the hippocampus and prefrontal cortex. The antidepressive pathways
involve the monoamines noradrenaline (NA) and 5-hydroxytryptamine (5-HT), which
act on G protein coupled receptors, and the brain-derived neurotrophic factor
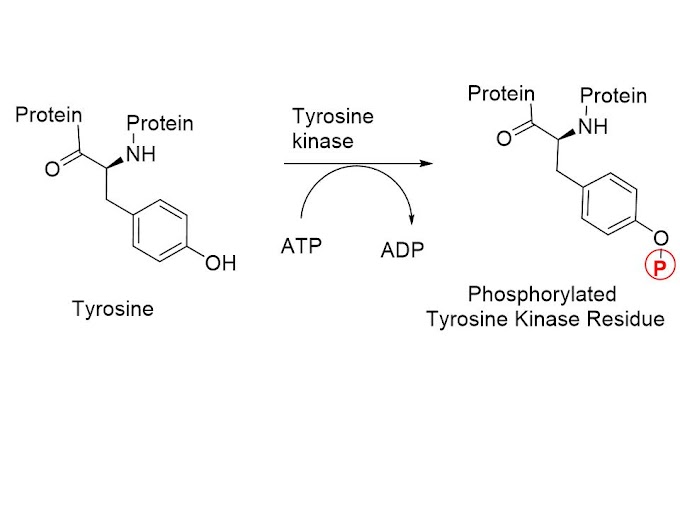
(BDNF), which acts on a kinase-linked receptor (TrkB), switching on genes that
protect neurons against apoptosis and also promote neurogenesis.
THE
MONOAMINE THEORY
The monoamine theory of depression, fist proposed by
Schildkraut in 1965, states that depression is caused by a functional deficit
of the monoamine transmitters, noradrenaline and 5-hydroxytryptamine (5-HT) at
certain sites in the brain, while mania results from a functional excess
NEUROENDOCRINE MECHANISM
→ Raised CRH levels are associated with stress and, in many cases, depression is preceded by periods of chronic stress. The plasma cortisol concentration is usually high in depressed patient.
→Hypothalamic neurons controlling pituitary function receive noradrenergic and 5-HT inputs, which control the discharge of these cells. Hypothalamic cells release corticotrophin-releasing hormone (CRH), which stimulates pituitary cells to secrete adrenocorticotrophic hormone (ACTH), leading in turn to cortisol secretion.
→ CRH concentrations in the brain and cerebrospinal fluid of depressed patients are increased. Therefore CRH hyperfunction, as well as monoamine hypofunction, may be associated with depression.
TROPHIC EFFECTS AND NEUROPLASTICITY
Depressive behaviour is often associated with a reduction in brain-derived neurotrophic factor (BDNF) expression and treatment with antidepressants elevates BDNF levels.
Lowered levels of BDNF or malfunction of its receptor, TrkB, plays a significant role in the pathology of Depression.
Antidepressant treatment may reduce glutamate release and depress NMDA receptor function. Changes in glutamatergic neurotransmission may also be involved in depression.
Classification of Antidepressant
Drugs
I) Inhibitors of
monoamine uptake:
1. Selective serotonin reuptake inhibitors (SSRIs) E.g. Fluoxetine, Fluvoxamine,
Paroxetine, Sertraline, Citalopram, Escitalopram, Dapoxetine
2. Serotonin and noradrenaline reuptake inhibitors (SNRIs) E.g. Venlafaxine, Duloxetine
3. Tricyclic antidepressants (TCAs):
A. NA + 5-HT reuptake inhibitors: E.g. Imipramine, Amitriptyline, Trimipramine, Doxepin, Dothiepin, Clomipramine
B. Predominantly NA reuptake inhibitors: E.g. Desipramine, Nortriptyline, Amoxapine, Reboxetine
II) Noradrenaline reuptake inhibitors (e.g. bupropion, reboxetine, atomoxetine).
The herbal preparation St John’s wort, whose main active ingredient is hyperforin: it has similar clinical efficacy to most of the prescribed antidepressants. It is a weak monoamine uptake inhibitor but also has other actions
III) Monoamine receptor antagonists
Drugs such as mirtazapine, trazodone, mianserin are non-selective and inhibit a range of amine receptors including α2 adrenoceptors and 5-HT2 receptors. They may also have weak effects on monoamine uptake.
IV) Monoamine oxidase inhibitors (MAOIs)
• Irreversible, non-competitive inhibitors (e.g. phenelzine, tranylcypromine),
which are nonselective with respect to the MAO-A and -B subtypes.
• Reversible, MAO-A-selective inhibitors (e.g. moclobemide).





0 Comments